Sloan Kettering Institute Director Joan Massagué (right), pictured here with laboratory member Karuna Ganesh, has been studying the biology behind cancer metastasis for nearly two decades.
Cancer metastasis occurs when cells break off from a tumor, spread through the bloodstream or lymph vessels, and establish themselves in another part of the body. Many primary tumors can be eliminated with surgery, chemotherapy, and other treatments. Once cancer is widely disseminated, however, it becomes much harder to stop. This is especially true when it spreads to vital organs, such as the lungs, liver, or brain. In fact, it is widely estimated that 90% of cancer deaths are due to metastatic disease rather than the original tumor.
Memorial Sloan Kettering cancer biologist Joan Massagué, Director of the Sloan Kettering Institute, has been studying the biology behind cancer metastasis for nearly two decades. His work has led to groundbreaking discoveries about the genes that influence how tumors interact with their environment. These genes allow cancer cells to enter and exit the bloodstream and lymphatic system so they can colonize various organs.
What is cancer metastasis?
Cancer metastasis occurs when cells break off from a tumor, spread through the bloodstream or lymph vessels, and establish themselves in another part of the body. Learn more about how cancer metastasis works.“It’s difficult for cancer cells to seed new tumors in other parts of the body,” Dr. Massagué says. “To get through all the barriers that are waiting for them when they leave the mother ship, the ones that survive have to be tougher than the average cancer cell. This explains why these cells tend to be more aggressive and harder to treat.”
Residual Disease: Finding What’s Left Behind after Treatment
Much of Dr. Massagué’s current work is focused on latent metastasis, which is also called dormant metastasis or residual disease.
From the time a tumor first forms, it sheds cancerous cells. These cells may travel to other parts of the body, where they are able to evade detection for months, years, or even decades. Even after treatment for the primary tumor leaves a person cancer free, some of these cells may be left behind.
“This is not in itself cause for alarm,” he notes. “Even though these cells are pathogenic, that doesn’t mean the person has active disease.” He uses the analogy of having germs on your hands: Just because you’ve picked up dangerous microbes from touching a doorknob, it doesn’t mean you will automatically get sick.
“For an infection to occur, germs must break through the barrier of immunity. Cancer has to break through that barrier, too,” says Dr. Massagué, who also leads the Alan and Sandra Gerry Metastasis and Tumor Ecosystems Center.
Utilizing the Immune System to Fight Cancer Metastasis
In the same way that the immune system protects us from infection, it also detects and kills the vast majority of cancer cells that are circulating through our bodies. “One important research effort is to find ways to help the immune system kill the cells that remain, so we can decrease the probability that a few pathogenic cells will break through,” Dr. Massagué says.
He calls the increased focus on immunotherapy research in recent years “an incredible opportunity to learn more about the confrontation between the immune system and cancer.”
The immune cells called natural killer cells are one of the first lines of defense against both cancer and infection. But they have a hard time detecting cells that are not actively dividing. “It makes sense,” Dr. Massagué says. “You want to put out the fires that are already burning. We need better ways to find and eliminate cells that are not yet growing but could cause trouble in the future. When disease is not a problem, that may be when you can attack it most efficiently.”
Building a Tool Kit to Research Metastasis
Dr. Massagué says there are several things needed to tap the potential for this research. “The good news is that we don’t need to invent a new approach,” he notes. “We just need to apply the methods we’ve already developed and turn them to focus on the problem of metastasis.”
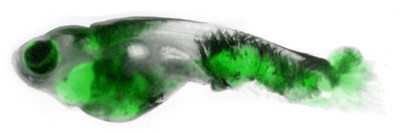
Animal models that closely replicate what happens in the human body are important for studying metastasis. Although research done in a dish or test tube is also essential, there are certain aspects of latent disease that are best studied in animals, especially mice and zebrafish. In addition, large numbers of samples collected from patients are needed. These include samples from primary tumors, metastatic tumors, and circulating tumor DNA. From these, researchers can analyze and sequence the DNA from tumors at all stages and look for patterns.
Because of the resources they have and the degree to which they collaborate with one another and the doctors on MSK’s various disease management teams, researchers at SKI are uniquely positioned to take advantage of these tools. In particular, Dr. Massagué notes the expertise in the Cancer Biology and Genetics, Computational and Systems Biology, and Immunology programs in tackling many of these questions. “This is exciting work, and an exciting time to be doing it,” he concludes.