Scientists at MSK are working to understand how cancer cells hide out in the body, sometimes for years at a time.
Consider this scenario: A man has surgery to remove a tumor in his kidney. No additional cancer is detected and the man remains cancer free for 29 years. Then, without warning, the cancer returns somewhere else in his body.
This case is real, reported last week in the journal Oncology Times.
Although the three-decade time interval is unusual, the phenomenon of cancer returning after successful initial treatment is all too common. Roughly 25% of women with HER2-positive breast cancer will experience a recurrence of their disease following surgery and chemotherapy. For lung cancer patients the numbers are worse — 50% will see their cancer come back.
“From the time a tumor begins to form until it is surgically removed, it is shedding tumor cells into the body,” says Joan Massagué, Director of the Sloan Kettering Institute and Executive Director of the Alan and Sandra Gerry Metastasis and Tumor Ecosystems Center at Memorial Sloan Kettering. “Most of these cells die, but a few may not.”
These stragglers can go into hiding, only to flare up later somewhere else — a phenomenon termed latent (or dormant) metastasis.
In a paper published today in Cell, Dr. Massagué and colleagues describe how they created a new model to understand latent metastasis and used it to uncover — for the first time — the mechanisms that underlie cancer’s stealth mode.
“Understanding latent metastasis is the biggest untapped opportunity to have a major impact on cancer,” says Dr. Massagué. “But so far, no one has been able to tackle it.”
Modeling Metastasis
It is hard enough for scientists to find latent cancer cells in the body, let alone identify what makes them tick. “People have known for years that latent metastasis exists, but there has been no good way to study it,” says Srinivas Malladi, a postdoctoral fellow in Dr. Massagué’s lab who is the paper’s first author and who spent six years developing the model and putting it to use.
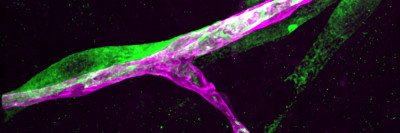
He started with tumor cells obtained from patients with early-stage breast and lung cancers, which he labeled with a fluorescent tag. He then injected these cells into mice and waited several months. Nearly all of the transplanted cells died, but a few survived. He found them hiding in the lungs and kidneys. He called these persistent survivors latency competent cancer (LCC) cells.
With these LCC cells in hand, Dr. Malladi could begin to investigate what made them so stealthy.
The first clue came from looking at the proteins the cells make. He found that, in this respect, LCC cells behave a lot like stem cells, which divide periodically to repair our tissues. This stem-like quality, Dr. Malladi says, helps to explain the LCC cells’ ability to divide and seed distant organs.
More tantalizing, he found that a proportion of these cells produce a protein (called a WNT inhibitor) that blocks cell division, forcing them into a state of suspended animation. This slowed-down growth is central to the cells’ ability to survive in the body without detection.
Immune Evasion
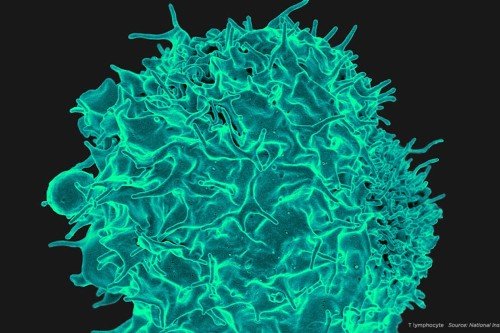
By not dividing, the LCC cells become less conspicuous to an important class of immune cells called natural killer (NK) cells that routinely patrol the body, looking for signs of danger.
“The job of NK cells is to sniff out anything that looks funny — like cancer cells — and kill it,” Dr. Massagué says.
But when cells aren’t dividing, they don’t make the molecules that NK cells detect, and so the NK cells ignore them.
What’s more, most chemotherapies kill only dividing cells, which means that non-dividing LCCs are spared.
Together, these facts explain why most LCC cells are eliminated from the body but a few can survive. Over time, the cells may acquire additional mutations that allow them to escape immune patrol completely and cause a cancer recurrence.
A Call to Arms
The idea that the immune system holds latent cancer in check is not new. The starkest example of this immune surveillance comes from the land of organ transplantation: Patients receiving an organ from a donor who previously had cancer but was thought to be cured sometimes come down with the disease. (Organ transplant recipients are given heavy doses of immune suppressants to prevent organ rejection, which apparently allows latent metastases to spring to life.) But up until now, the mechanism through which latent cancer and the immune system battle it out had remained mysterious.
This new work from Dr. Massagué’s lab helps to clear up the mystery and opens the door to new treatment options that may succeed where others have failed.
An effective strategy to target latent cancer cells might be to prod them into producing the molecules that would alert NK cells to their presence, Dr. Massagué says. To that end, he and his team plan to work with immunologists to study these cells further and hopefully develop potential therapies that could be available within the decade.