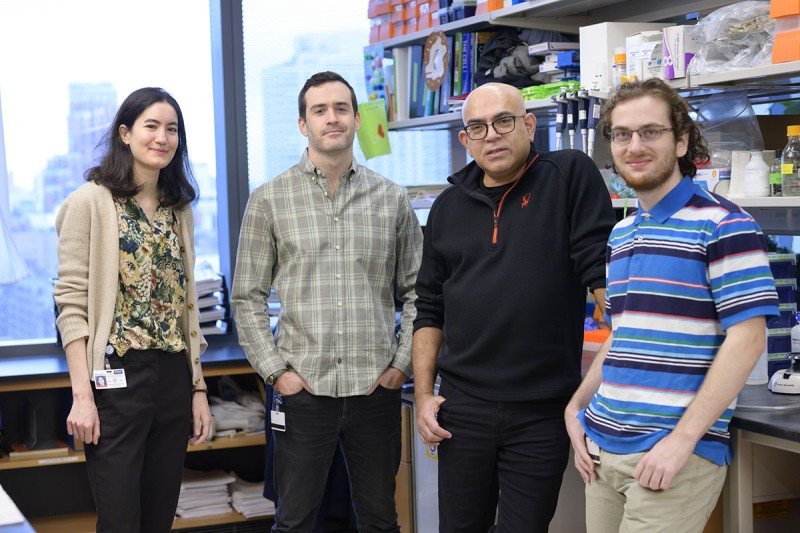
Immunologist Jayanta Chaudhuri (second from right) with members of his lab (from left) graduate student Kalina Belcheva, postdoctoral fellow Teddy Yewdell, and graduate student Ryan Smolkin
When Sloan Kettering Institute (SKI) postdoctoral fellow William “Teddy” Yewdell embarked on a new research project in 2015, he didn’t know it ultimately could help in fighting a global pandemic. Dr. Yewdell studies how the immune system responds to viruses, including how to optimize the timing between vaccine shots. This research has the potential to impact future COVID-19 vaccination strategies.
In a paper published November 9, 2021, in Cell Reports, Dr. Yewdell and his research mentor, SKI immunologist Jayanta Chaudhuri, report that they used a lab model of mice infected with influenza A virus, otherwise known as flu, to study how the body produces antibodies against respiratory viruses after infection or vaccination. Their research reveals that the body can mount a response to viral infection for longer than previously thought.
This finding suggests that the first and second vaccine doses for COVID-19 potentially could be spaced further apart, although much more research is needed before changing the current vaccination schedules.
“The point of getting a second shot is to reenergize the immune system to make more antibodies against a virus,” Dr. Yewdell says. “We’re finding that it’s important to study this process more carefully so we can ensure that the second shot provides the greatest benefit.” Both the Pfizer-BioNTech and Moderna vaccines currently in wide use in the United States require two shots spaced three or four weeks apart. Federal health officials now recommend people receive a booster dose six or more months after their initial vaccination to help maintain their immunity.
Studying Immune Cell ‘Factories’
Dr. Chaudhuri’s lab in the SKI Immunology Program focuses on how antibody-based immunity, also known as humoral immunity, develops. Two main cell types are vital to humoral immunity: plasma cells, which make antibodies, and memory B cells, which are dormant sentinels that prepare the body for future infections. Both cell types contribute to long-lasting protection from viruses.
With some viruses, including both the flu and SARS-CoV-2 (the virus that causes COVID-19), structures called germinal centers form inside the lymph nodes and spleen after either infection or vaccination. “These germinal centers are the factories that turn out the memory B cells,” Dr. Chaudhuri says. “They also make changes to the B cells, which allows the immune system to adapt to variants that are slightly different from the original virus.”
In the new study, the investigators looked at the germinal centers that formed in mice infected with flu. These germinal centers were located in the lymph nodes near the lungs. The team found that the germinal centers could persist for up to five months after infection, much longer than expected. Additionally, the germinal centers constantly produced memory B cells throughout that time. The findings indicate that initial exposure to respiratory viruses may lead to a longer-lasting immune response than previously thought.
“In countries where the first two COVID-19 shots were spaced further apart, there have been some indications that people seem to have higher protection,” Dr. Yewdell says. “Our study suggests why it might be beneficial to have more time between the first and second shots — it allows recipients to get maximum benefit from the first shot.”
A Valuable Model for Future Research
Historically, memory B cells have been challenging to study, in part because they are produced at a low frequency and can be difficult to track. Recently, mouse models of viral infection have made it easier for scientists to study how these cells form in mammals — including humans.
A key part of the new study is the identification of new genes that may regulate how long memory B cells stick around. The ability to identify long-lived memory B cells after flu infection, combined with single-cell analysis, allowed the investigators to identify which genes may play a role in prolonging the life span of memory B cells.
“We know that not all people respond the same way to vaccination, and this may be due to differences in these genes,” Dr. Chaudhuri adds. “One of the values of doing this research in mice is that we can make modifications that help us understand the role of genes and how they affect the behavior of immune cells.”
“What the field of immunology needs now is better tools to continue asking these kinds of questions,” Dr. Yewdell concludes. “And that’s what we’re working on through our research.”
- Sloan Kettering Institute scientists are studying how the immune system responds to infection with respiratory viruses.
- This research has potential implications for the timing of COVID-19 vaccines.
- Findings in mice suggest that the first and second doses of the vaccine could be spaced further apart.
- More research is needed before changes are made to vaccination schedules.