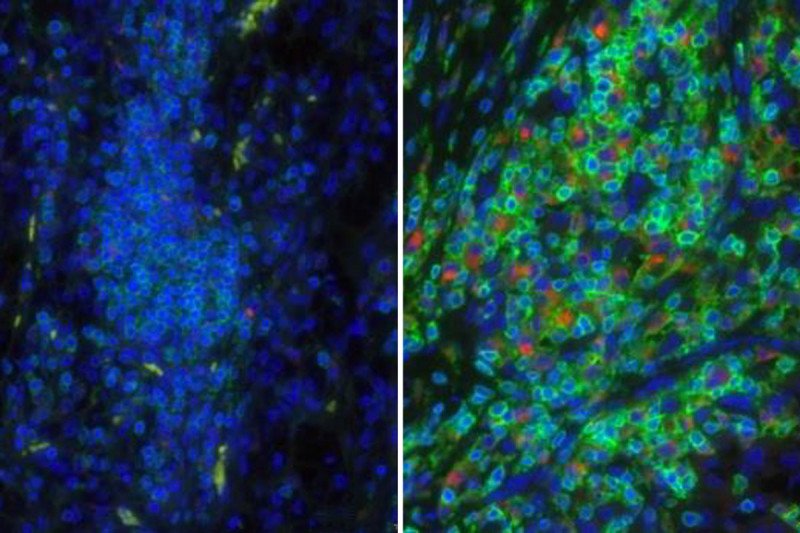
These fluorescently labeled sections of kidney tumors show immune cells (green) and macrophages (red). On the left is a tumor from a person who responded to targeted therapy, showing few immune cells and macrophages. On the right is a tumor from a non-responder, showing many immune cells and macrophages.
If cancer is like a weed that sprouts from a seed, then the tumor microenvironment is like the soil that nurtures its growth. Some microenvironments provide fertile ground for tumor growth, while others can be more inhospitable.
New research from scientists at Memorial Sloan Kettering shows that the tumor microenvironment in kidney cancer also strongly influences how well the disease responds to targeted cancer drugs.
The findings emerge from sophisticated genetic analyses of tumor samples taken from people with metastatic clear cell renal cell carcinoma, a type of kidney cancer that has spread to other locations in the body. These individuals all participated in a clinical trial of two targeted drugs: sunitinib (Sutent®) and pazopanib (Votrient®). The trial ended in 2013. A total of 409 patients were included in the analyses.
According to Ari Hakimi, the MSK surgeon-scientist who led the new study, the data identified distinct groups of patients who respond differently to the drugs. “One cluster of patients responded very well to the medications, while another cluster responded very poorly,” he says. “When we analyzed the gene expression of tumors in these clusters, we were able to determine that factors in the tumor microenvironment were making the crucial difference.”
Matching patients to drugs on the basis of these local factors, he says, could be one way to personalize treatments to make them more effective.
This sort of careful molecular analysis is a strength of MSK’s Immunogenomics and Precision Oncology Platform (IPOP), of which Dr. Hakimi is a member. IPOP is led by MSK physician-scientist Timothy Chan. Its goal is to identify the genetic and molecular reasons why people do and do not respond to particular types of cancer drugs, with a focus on immunotherapy. Drs. Hakimi and Chan are co-corresponding authors on the new study, which was published on January 8 in the journal Cancer Discovery.
Digging in the (Genetic) Dirt
The investigators’ genetic analyses revealed that there were two main variables affecting patients’ responses to treatment. One was the level of expression of genes involved in new blood vessel growth (angiogenesis). The other was the number of immune cells present in and around the tumor.
The former finding was not entirely surprising, since the drugs tested in the clinical trial are thought to specifically interfere with angiogenesis. They are believed to work by cutting off the tumor’s blood supply.
The latter finding was more unexpected. “The poorly responding tumors showed signs of a very robust immune response,” Dr. Hakimi says. “That was somewhat surprising to us, and we spent most of our time in this study trying to identify what these immune cells are and what they are doing.”
By analyzing both specific genetic markers and sections of tumor tissue, they were able to see that immune cells called macrophages predominated in the poorly responding cluster. More specifically, the macrophages were ones that made a molecule called PD-L1. This is a protein that acts as a brake on immune cells. When bound to another molecule called PD-1, it shuts down immune responses.
“The presence of these macrophages tells us that the body’s immune system is trying to fight the cancer, but the immune cells are basically paralyzed and cannot do their job,” Dr. Hakimi says.
Lessons for Immunotherapy and Beyond
Though the clinical trial did not involve immunotherapy drugs, the new data are relevant to this form of treatment. They suggest that people in the macrophage-predominating cluster would do well on immunotherapy drugs called checkpoint inhibitors. These medications are designed to release the brakes on immune cells.
But there’s more to the results than this. They also suggest that whatever treatment a person with kidney cancer is receiving — be it an immunotherapy drug or a targeted therapy — the tumor microenvironment matters and must be taken into account.
This conclusion is underscored by the finding that the two targeted drugs tested in the trial, sunitinib and pazopanib, differed in the extent to which macrophages affected the response.
“I think that’s the main lesson of our study,” Dr. Hakimi says. “As we begin to bring immunotherapy drugs more to the front line of therapy, we still have to think about what combinations of drugs are appropriate for particular patients, based on the unique microenvironment of their tumors.”
He adds, “You can’t just give one drug and expect all people to respond the same.”