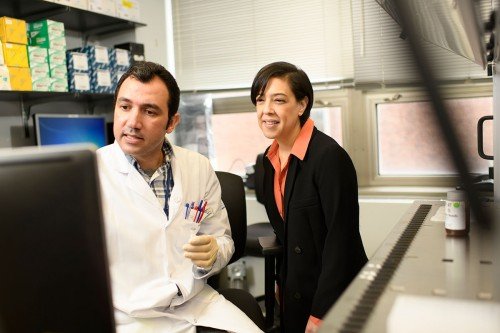
MSK-IMPACT™, a diagnostic test for cancer, has provided research data on the mutations found in more than 50,000 tumors. Shown here is the Marie-Josée & Henry R. Kravis Center for Molecular Oncology, where the test is performed.
A major effort in cancer research is the search for driver mutations in tumors. These mutations are changes in a gene’s DNA that play a direct role in the growth of cancer. They are different from passenger mutations, which are genetic changes found in tumors that don’t have anything to do with the cancer: Those are just along for the ride.
Figuring out which tumor mutations are drivers is important because they help provide an understanding of how and why tumors grow. Identifying driver mutations also helps researchers design treatments and helps doctors predict how a person’s cancer is likely to behave.
But according to a study published by Memorial Sloan Kettering researchers in Nature on May 27, the strategy of focusing on driver mutations may be more complicated than previously thought. It turns out that nearly a quarter of all tumors have two different mutations in the same gene that are contributing to the formation of an individual cancer.
“We’ve seen this phenomenon here and there before, but until now we had no idea how common it was,” says MSK computational oncologist Barry Taylor, one of the study’s two senior authors. “The harder we looked, the more clearly we saw it.”
A Surprisingly Common Occurrence
In every cell of our bodies, we have two copies of each gene. One comes from our mother and the other from our father. When one copy of a gene develops a mutation — either by chance or due to exposure to something harmful like UV light, radiation, or tobacco smoke — the other copy is there to potentially make up for the loss. If there is a mutation in the second copy, that’s when trouble can start: If both copies of a gene are mutated, it can send the cell down the road toward becoming cancerous. These multiple mutations, also called composite mutations, were known to occur with a class of genes called tumor suppressors, where the double mutation effectively cripples the function of both copies of a gene and can lead to cancer.
But it turns out that another type of composite mutation that hasn’t been well understood is much more common than expected: It occurs when two different mutations affect the same copy of a gene. Here, the two mutations work together to produce a mutant protein with new, unexpected functions. This situation can lead to the formation of oncogenic proteins — those that drive cancer growth.
“In a way, we’re looking at a phenomenon that’s been staring people in the face for a long time,” says MSK computational oncologist Ed Reznik, the paper’s other senior author. “I credit graduate student Alex Gorelick, who was working in both my and Barry’s labs, with coming up with the idea to look at how common composite mutations are and what they may mean.” Mr. Gorelick is first author on the Nature paper.
The Power of Data
The team was able to make this discovery thanks to data from MSK-IMPACT™, a diagnostic test that helps match people with cancer to the best treatment based on the genetic changes in their tumors. This test, which has been used since 2014, has now analyzed more than 50,000 tumors, giving researchers a lot of data to work with.
“One special thing about MSK-IMPACT data is that it’s very deep and contains a lot more information than other sequencing platforms,” Dr. Reznik says. “That makes it well suited to doing this kind of detailed analysis.”
From Discovery to Understanding
Now that the researchers know about composite mutations, the next step is to determine what they might mean for individual cancers. One study that came out last year in Science, published by MSK cancer biologist Maurizio Scaltriti and colleagues, found that breast cancers with composite mutations in the gene PIK3CA may respond better to targeted therapy than breast cancers in which only one PIK3CA mutation is present.
However, with other cancers and other mutations, it’s possible that composite mutations may make them harder to treat.
“There’s still so much we don’t understand about composite mutations. Rather than creating frustration, knowing of their existence leads to new opportunities,” concludes Dr. Taylor, who is an Associate Director of the Marie-Josée & Henry R. Kravis Center for Molecular Oncology. “This gives us a tremendous opportunity to look at the function of these mutations in a different way and learn something fundamental about cancer genes that we may not have appreciated before.”