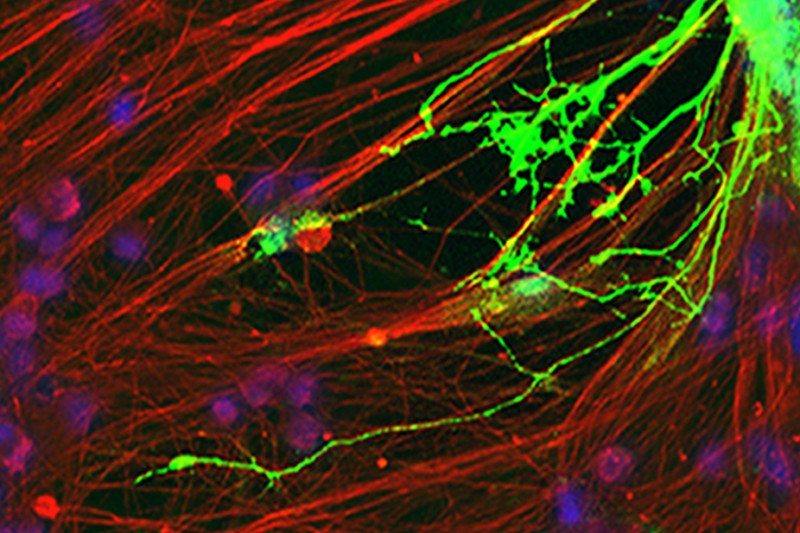
This image shows the fibrous extensions of a nerve cell (red) and an oligodendrocyte (green) growing on top of the nerve cell. The oligodendrocyte was generated in the lab by stem-cell engineering. Like natural oligodendrocytes in the brain, the engineered cell is capable of coating nerve fibers with myelin.
Here at Memorial Sloan Kettering and elsewhere, scientists are cultivating the art and science of manipulating embryonic stem cells — the immature cells from which all the body’s organs and tissues develop — to form nerve cells, muscle cells, insulin-producing cells, and essentially any cell type of interest.
Our investigators have used stem-cell engineering to create nerve cells that might be used to treat Parkinson’s, and have also developed advanced tools for research into melanoma, pancreatic cancer, a rare brain tumor, and other diseases.
Today, in an article published in the journal Cell Stem Cell, an MSK research team reports on another potential use of the technology: as a way to heal radiation-induced brain injury.
“Some cancer patients who receive radiation to the brain eventually experience cognitive problems, such as learning or thought-processing difficulties, or reduced motor skills,” says stem-cell scientist and neurosurgeon Vivian Tabar, who led the study. “And often the damage is permanent.”
She adds that there’s a growing need to find ways to alleviate these complications. “As we get better at treating some cancers and our patients live longer, it’s becoming increasingly obvious that many of them suffer from long-term quality-of-life issues.”
The researchers turned stem cells into young central nervous system cells that can mature into oligodendrocytes, which support nerve cells. After exposing rats to brain radiation, they transplanted the engineered oligodendrocytes into the animals’ brains. The cells repaired some of the radiation injury and helped the animals recover a number of brain functions that had been compromised by the treatment.
The Late Side Effects of Brain Radiation
Radiation to the brain is used to treat primary or metastatic brain tumors as well as to prevent the spread of small cell lung cancer or leukemia to the brain. The treatment can be very effective in terms of managing the cancer, but for some patients, it impairs long-term quality of life, even when done with cutting-edge methods such as stereotactic radiosurgery.
The severity and types of complications vary depending on the amount of radiation and other therapies used, as well as the patient’s age. “For example,” Dr. Tabar explains, “learning difficulties are more serious in children and may lessen their chance of achieving higher education or maintaining a job in the future.”
The problems often don’t show up until months or years after cancer treatment has ended, and their underlying causes are complex.
Rats in a Box
In the study, the researchers focused on one of the best-understood mechanisms of radiation-induced brain damage: the loss of oligodendrocytes. These cells produce a substance called myelin, which forms a supple casing around nerve fibers. Like the plastic coating around an electric copper wire, the myelin sheath insulates nerve cells and allows them to transmit their signals very quickly.
In people whose oligodendrocytes have been depleted by radiation, some brain functions may weaken as myelin production drops and nerves are insufficiently coated.

Many nerve cells in the brain are coated with myelin, a casing that insulates the nerve and allows it to transmit signals very quickly. In some myelin-coated nerves, signals travel as fast as 200 miles per hour.
The researchers devised a technique to generate oligodendrocytes from human embryonic stem cells in the large amounts needed for transplantation. They also developed a rat model to study the neurological side effects of radiation to the brain. “We gave the rats repeated doses of radiation and showed that they developed complications similar to those seen in cancer patients,” explains postdoctoral fellow Jinghua Piao, the first author of the study.
For example, in one of the experiments she used to test cognition, Dr. Piao put the rats in a box together with a few items. After some time, she introduced a new item into the box and observed the rats’ behavior. Compared with a control group, those rats that had received radiation were less capable of distinguishing the new item from the more-familiar ones.
Hope for Clinical Translation
Next, the researchers transplanted the engineered oligodendrocytes into the brains of these rats. “The cells were able to spread across most of the brain, integrate into the tissue, and add myelin to the nerves,” Dr. Piao says.
“And not only did the grafted oligodendrocytes repair the physical damage,” Dr. Tabar adds, “they also helped the rats improve a number of brain functions such as learning, memory, and balance.”
The findings suggest the technology might be safe if used as therapy. “No animals developed tumors or other complications as a result of the transplant, and the cells appeared to behave like natural oligodendrocytes,” she says, adding that a lot of work remains before the method can be tested safely in patients.
If the research eventually makes it into the clinic, it could offer promising treatment strategies. Stem cell–derived oligodendrocytes could potentially be given to patients who undergo brain radiation to alleviate damage. The approach could improve patients’ quality of life and also extend the use of radiation to some patients for whom the potentially curable treatment is presently too risky.
“Sometimes brain radiation can’t be used, especially in children, because the side effects are so damaging,” Dr. Tabar explains. “But with a way to fix the problem, the risks could become more manageable.”